Hover to pan and click to magnify. Click again to pan at full screen.
Jonathan Jamito, MD
Jonathan Jamito, MD
Icahn School of Medicine at Mount Sinai Morningside and Mount Sinai West
ABSTRACT:
Case Presentation
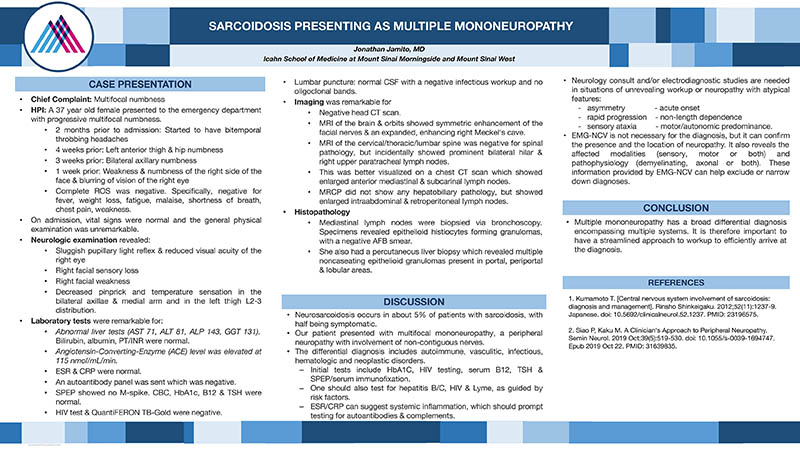
A 37 year old female presented to the emergency department with progressive multifocal numbness. 2 months prior to admission she started to have bitemporal throbbing headaches, followed by left anterior thigh & hip numbness, followed by bilateral axillary numbness, and then, weakness & numbness of the right side of the face & blurring of vision of the right eye. On admission, vital signs were normal and the general physical examination was unremarkable. Neurologic examination revealed a sluggish pupillary light reflex & reduced visual acuity of the right eye, right facial sensory loss, right facial weakness, decreased pinprick and temperature sensation in the bilateral axillae & medial arm and in the left thigh L2-3 distribution. Laboratory studies revealed abnormal liver tests (AST 71, ALT 81, ALP 143, GGT 131). Bilirubin, albumin, PT/INR were normal. An Angiotensin-Converting-Enzyme (ACE) level was elevated at 115 nmol/mL/min. ESR & CRP were normal. An autoantibody panel was sent which was negative. SPEP showed no M-spike. HbA1c, B12 & TSH were normal. A lumbar puncture yielded normal CSF with a negative infectious workup and no oligoclonal bands. HIV test & QuantiFERON TB-Gold were negative. Head CT scan was negative. MRI of the brain & orbits showed symmetric enhancement of the facial nerves & an expanded, enhancing right Meckel's cave. MRI of the cervical/thoracic/lumbar spine was negative for spinal pathology, but incidentally showed prominent bilateral hilar & right upper paratracheal lymph nodes. This was better visualized on a chest CT scan which showed enlarged anterior mediastinal & subcarinal lymph nodes. MRCP did not show any hepatobiliary pathology, but showed enlarged intraabdominal & retroperitoneal lymph nodes. The mediastinal lymph nodes were biopsied via bronchoscopy. Specimens revealed epithelioid histiocytes forming granulomas, with a negative AFB smear. She also had a percutaneous liver biopsy which revealed multiple noncaseating epithelioid granulomas present in portal, periportal & lobular areas. The final diagnosis was sarcoidosis with neurologic and hepatic involvement.
Discussion
Neurosarcoidosis occurs in about 5% of patients with sarcoidosis, with half being symptomatic. Our patient presented with multifocal mononeuropathy, a peripheral neuropathy with involvement of non-contiguous nerves. The differential diagnosis includes autoimmune, vasculitic, infectious, hematologic and neoplastic disorders. Initial tests include HbA1C, HIV testing, serum B12, TSH & SPEP/serum immunofixation. One should also test for hepatitis B/C, HIV & Lyme, as guided by risk factors. ESR/CRP can suggest systemic inflammation, which should prompt testing for autoantibodies & complements. Neurology consult and/or electrodiagnostic studies are needed in situations of unrevealing workup or neuropathy with features of asymmetry, acute onset, rapid progression, non-length dependence, sensory ataxia, motor/autonomic predominance. EMG-NCV is not necessary for the diagnosis, but it can confirm the presence and the location of neuropathy. It also reveals the affected modalities (sensory, motor or both) and pathophysiology (demyelinating, axonal or both). These information provided by EMG-NCV can help exclude or narrow down diagnoses.
Conclusions
Multiple mononeuropathy has a broad differential diagnosis encompassing multiple systems. It is therefore important to have a streamlined approach to workup to efficiently arrive at the diagnosis.
References
1. Kumamoto T. [Central nervous system involvement of sarcoidosis: diagnosis and management]. Rinsho Shinkeigaku. 2012;52(11):1237-9. Japanese. doi: 10.5692/clinicalneurol.52.1237. PMID: 23196575.
2. Siao P, Kaku M. A Clinician's Approach to Peripheral Neuropathy. Semin Neurol. 2019 Oct;39(5):519-530. doi: 10.1055/s-0039-1694747. Epub 2019 Oct 22. PMID: 31639835.

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE