Hover to pan and click to magnify. Click again to pan at full screen.
Diego R. Mazzotti, PhD, Timo Leppänen, PhD, Scott Sands, PhD, Juha Töyräs, PhD, Andrew Wellman, MD, PhD, Antti Kulkas, PhD, Susan Redline, MD, Tuomas Karhu, MSc, Ali Azarbarzin, PhD
Diego R. Mazzotti, PhD, Timo Leppänen, PhD, Scott Sands, PhD, Juha Töyräs, PhD, Andrew Wellman, MD, PhD, Antti Kulkas, PhD, Susan Redline, MD, Tuomas Karhu, MSc, Ali Azarbarzin, PhD
Division of Medical Informatics, Department of Internal Medicine, University of Kansas Medical Center, Kansas City, KS, USA; Department of Applied Physics, University of Eastern Finland, Kuopio, Finland; Diagnostic Imaging Center, Kuopio University Hospital, Kuopio, Finland;
Division of Sleep and Circadian Disorders, Brigham and Women's Hospital and Harvard Medical School, Boston, MA; School of Information Technology and Electrical Engineering, The University of Queensland, Brisbane, Australia; Department of Clinical Neurophysiology, Seinäjoki Central Hospital, Seinäjoki, Finland
BACKGROUND
• Obstructive sleep apnea (OSA) is a common and heterogeneous sleep disorder and established risk factor for cardiovascular (CV) diseases
• The apnea-hypopnea index (AHI) has been used to characterize OSA severity. However, this metric is limited in providing information about CV disease risk.
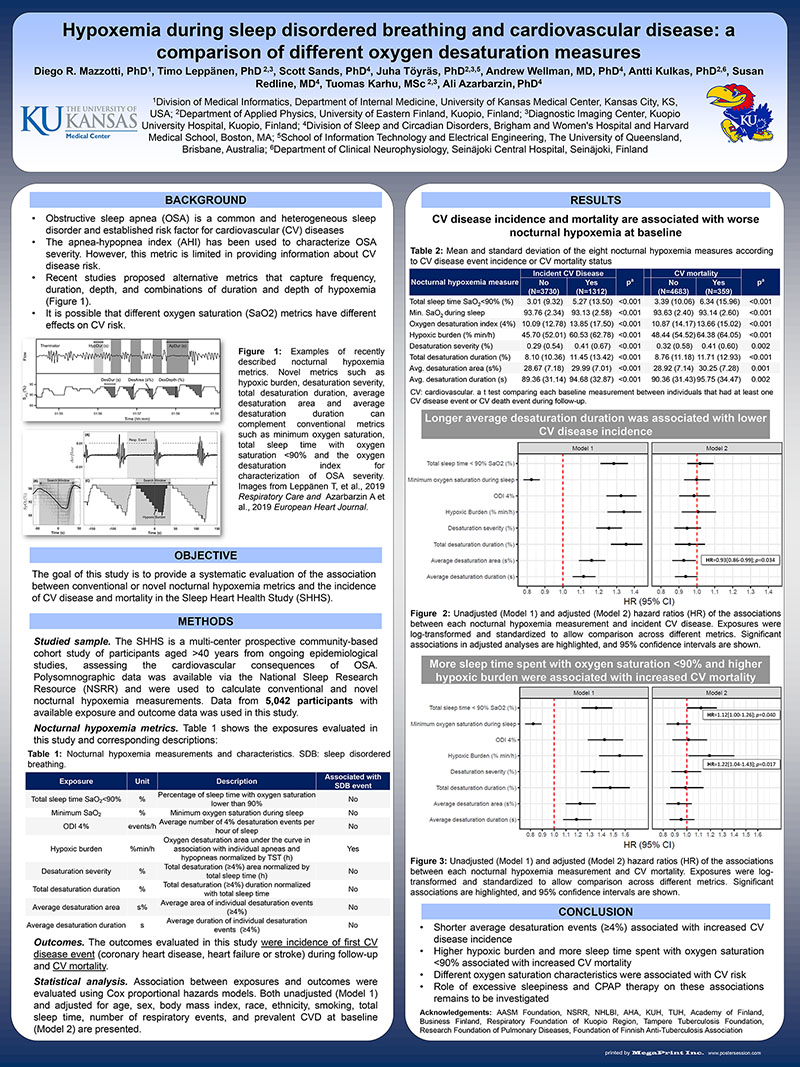
• Recent studies proposed alternative metrics that capture frequency, duration, depth, and combinations of duration and depth of hypoxemia (Figure 1).
• It is possible that different oxygen saturation (SaO2) metrics have different effects on CV risk.
(View poster)
Figure 1: Examples of recently described nocturnal hypoxemia metrics. Novel metrics such as hypoxic burden, desaturation severity, total desaturation duration, average desaturation area and average desaturation duration can complement conventional metrics such as minimum oxygen saturation, total sleep time with oxygen saturation <90% and the oxygen desaturation index for characterization of OSA severity. Images from Leppänen T, et al., 2019 Respiratory Care and Azarbarzin A et al., 2019 European Heart Journal.
OBJECTIVE
The goal of this study is to provide a systematic evaluation of the association between conventional or novel nocturnal hypoxemia metrics and the incidence of CV disease and mortality in the Sleep Heart Health Study (SHHS).
METHODS
Studied sample. The SHHS is a multi-center prospective community‐based cohort study of participants aged >40 years from ongoing epidemiological studies, assessing the cardiovascular consequences of OSA. Polysomnographic data was available via the National Sleep Research Resource (NSRR) and were used to calculate conventional and novel nocturnal hypoxemia measurements. Data from 5,042 participants with available exposure and outcome data was used in this study.
Nocturnal hypoxemia metrics. Table 1 shows the exposures evaluated in this study and corresponding descriptions:
Table 1: Nocturnal hypoxemia measurements and characteristics. SDB: sleep disordered breathing.
(View poster)
Outcomes. The outcomes evaluated in this study were incidence of first CV disease event (coronary heart disease, heart failure or stroke) during follow-up and CV mortality.
Statistical analysis. Association between exposures and outcomes were evaluated using Cox proportional hazards models. Both unadjusted (Model 1) and adjusted for age, sex, body mass index, race, ethnicity, smoking, total sleep time, number of respiratory events, and prevalent CVD at baseline (Model 2) are presented.
RESULTS
CV disease incidence and mortality are associated with worse nocturnal hypoxemia at baseline
Table 2: Mean and standard deviation of the eight nocturnal hypoxemia measures according to CV disease event incidence or CV mortality status
(View poster)
Longer average desaturation duration was associated with lower CV disease incidence
(View poster)
Figure 2: Unadjusted (Model 1) and adjusted (Model 2) hazard ratios (HR) of the associations between each nocturnal hypoxemia measurement and incident CV disease. Exposures were log-transformed and standardized to allow comparison across different metrics. Significant associations in adjusted analyses are highlighted, and 95% confidence intervals are shown.
More sleep time spent with oxygen saturation <90% and higher hypoxic burden were associated with increased CV mortality
(View poster)
Figure 3: Unadjusted (Model 1) and adjusted (Model 2) hazard ratios (HR) of the associations between each nocturnal hypoxemia measurement and CV mortality. Exposures were log-transformed and standardized to allow comparison across different metrics. Significant associations are highlighted, and 95% confidence intervals are shown.
CONCLUSION
• Shorter average desaturation events (≥4%) associated with increased CV disease incidence
• Higher hypoxic burden and more sleep time spent with oxygen saturation <90% associated with increased CV mortality
• Different oxygen saturation characteristics were associated with CV risk
• Role of excessive sleepiness and CPAP therapy on these associations remains to be investigated
Acknowledgements: AASM Foundation, NSRR, NHLBI, AHA, KUH, TUH, Academy of Finland, Business Finland, Respiratory Foundation of Kuopio Region, Tampere Tuberculosis Foundation, Research Foundation of Pulmonary Diseases, Foundation of Finnish Anti-Tuberculosis Association
Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
