Hover to pan and click to magnify. Click again to pan at full screen.
Ryan Hawkins, Rishabh Gupta, Mary Champion, Martin Mainster, Radwan Ajlan
Ryan Hawkins, Rishabh Gupta, Mary Champion, Martin Mainster, Radwan Ajlan
Department of Ophthalmology, University of Kansas School of Medicine
Introduction
Macular holes form when there is a break in the central part of the
retina. The retina is the light-sensitive tissue in the back of the eye. The
macula provides the central part of the field of vision and is key in
overall visual acuity due to its high density of photoreceptor cells.
When a macular hole occurs, the central vision is distorted and
blurred(1). The formation of intraretinal cysts at the boarder of these
macular holes caused by traction of the vitreous as it pulls away from
the back of the eye can further exacerbate these symptoms--but could
also potentially suggest a more recent break in the macula, and thus
the potential for better recovery after repair.
It is estimated that 7.8 per 100,000 new persons develop macular hole
each year, 80% of which are unilateral(2). The risk is also almost two thirds
greater in women than in men. If left untreated, a macular hole
can progress and result in further impairment of the visual field. The
most common treatment for macular hole repair is surgical vitrectomy
where the vitreous is removed from inside the eye, coexisting epiretinal
membrane is peeled with or without the internal limiting membrane
removal. The use of Optical Coherence Tomography (OCT) is the current
gold standard imaging modality for diagnosis and management of
macular holes. The images provided by OCT allow for visualization of
the ten retinal layers and their densities(3).
Purpose
To determine if the number of pre-operative intraretinal cysts bordering
a macular hole (“border cysts”) and/or their spectral domain optical
coherence tomography (SD-OCT) optical density ratios are potentially
useful predictors of visual performance after the surgical repair of a full thickness
macular hole.
Methods
A retrospective chart review was performed on 375 patients who
underwent macular hole surgery at the University of Kansas Medical
Center over the past 10 years and had preoperative SD-OCT scans. Two
independent readers examined all available scans. Image-J software
was used to measure macular hole diameter, count border cysts and
determine the ratio of SD-OCT optical density within border cysts to
that of the overlying vitreous (ODR). Data collected included LogMAR
visual acuity for analysis using the equation [LogMAR VA = -log(decimal
acuity)] (4), age, gender, ODR and macular hole diameter. The institutional
review board of the University of Kansas School of Medicine approved
this study.
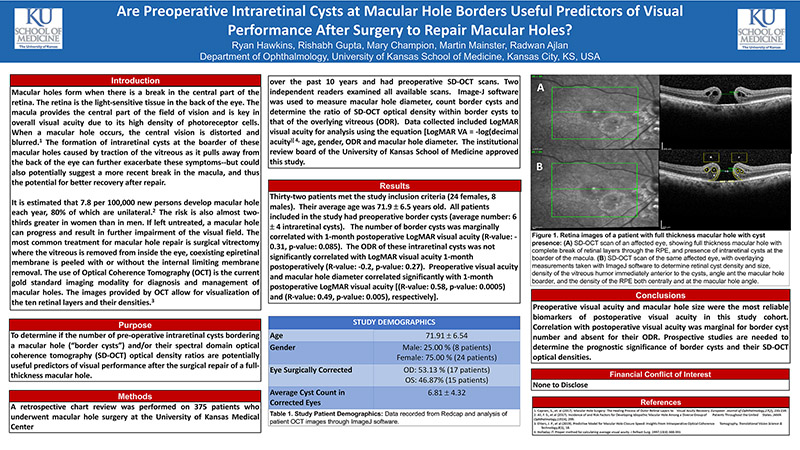
Results
Thirty-two patients met the study inclusion criteria (24 females, 8
males). Their average age was 71.9 ± 6.5 years old. All patients
included in the study had preoperative border cysts (average number: 6
± 4 intraretinal cysts). The number of border cysts was marginally
correlated with 1-month postoperative LogMAR visual acuity (R-value: -
0.31, p-value: 0.085). The ODR of these intraretinal cysts was not
significantly correlated with LogMAR visual acuity 1-month
postoperatively (R-value: -0.2, p-value: 0.27). Preoperative visual acuity
and macular hole diameter correlated significantly with 1-month
postoperative LogMAR visual acuity [(R-value: 0.58, p-value: 0.0005)
and (R-value: 0.49, p-value: 0.005), respectively].
Results
Are Preoperative Intraretinal Cysts at Macular Hole Borders Useful Predictors of Visual
Performance After Surgery to Repair Macular Holes?
Ryan Hawkins, Rishabh Gupta, Mary Champion, Martin Mainster, Radwan Ajlan
Department of Ophthalmology, University of Kansas School of Medicine, Kansas City, KS, USA.
(View poster)
Conclusions
Preoperative visual acuity and macular hole size were the most reliable
biomarkers of postoperative visual acuity in this study cohort.
Correlation with postoperative visual acuity was marginal for border cyst
number and absent for their ODR. Prospective studies are needed to
determine the prognostic significance of border cysts and their SD-OCT
optical densities.
Financial Conflict of Interest
None to Disclose
References
1. Caprani, S., et. al (2017). Macular Hole Surgery: The Healing Process of Outer Retinal Layers to Visual Acuity Recovery. European Journal of Ophthalmology,27(2), 235-239.
2. Ali, F. S., et al (2017). Incidence of and Risk Factors for Developing Idiopathic Macular Hole Among a Diverse Group of Patients Throughout the United States. JAMA
Ophthalmology,135(4), 299.
3. Ehlers, J. P., et al (2019). Predictive Model for Macular Hole Closure Speed: Insights From Intraoperative Optical Coherence Tomography. Translational Vision Science &
Technology,8(1), 18.
4. Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13(4):388-391

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE