Hover to pan and click to magnify. Click again to pan at full screen.
Dante Pennipede, Mary Champion, Martin Mainster, Radwan Ajlan
Dante Pennipede, Mary Champion, Martin Mainster, Radwan Ajlan
KU EYE, KU Medical Center
Introduction
Proliferative vitreoretinopathy (PVR) is the most common cause of rhegmatogenous retinal detachment surgery failure. It is a complication that occurs in 8-10% of patients undergoing primary retinal detachment (RD) repair.(1)(2) PVR is formed by an aberrant healing process brought forth by cellular proliferation surrounding the retina. This can occur through partial or full-thickness retinal breaks.(3) Retinal Pigment Epithelial cells, along with glial cells, form fibrocellular sheets, which contract, leading to significant retinal shortening. These contractile fibrocellular sheets may hold open retinal breaks, which lead to recurrent RD.(4)
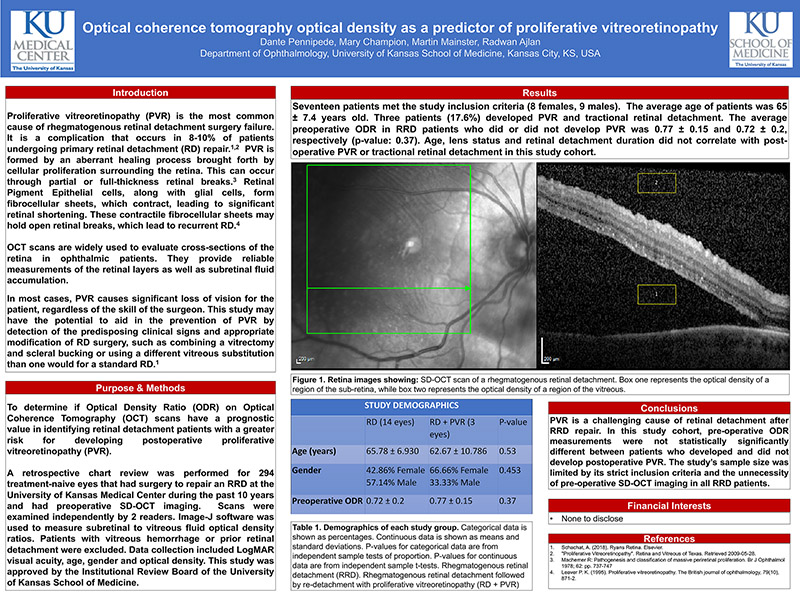
OCT scans are widely used to evaluate cross-sections of the retina in ophthalmic patients. They provide reliable measurements of the retinal layers as well as subretinal fluid accumulation.
In most cases, PVR causes significant loss of vision for the patient, regardless of the skill of the surgeon. This study may have the potential to aid in the prevention of PVR by detection of the predisposing clinical signs and appropriate modification of RD surgery, such as combining a vitrectomy and scleral bucking or using a different vitreous substitution than one would for a standard RD.(1)
Purpose & Methods
To determine if Optical Density Ratio (ODR) on Optical Coherence Tomography (OCT) scans have a prognostic value in identifying retinal detachment patients with a greater risk for developing postoperative proliferative vitreoretinopathy (PVR).
A retrospective chart review was performed for 294 treatment-naive eyes that had surgery to repair an RRD at the University of Kansas Medical Center during the past 10 years and had preoperative SD-OCT imaging. Scans were examined independently by 2 readers. Image-J software was used to measure subretinal to vitreous fluid optical density ratios. Patients with vitreous hemorrhage or prior retinal detachment were excluded. Data collection included LogMAR visual acuity, age, gender and optical density. This study was approved by the Institutional Review Board of the University of Kansas School of Medicine.
Results
Seventeen patients met the study inclusion criteria (8 females, 9 males). The average age of patients was 65± 7.4 years old. Three patients (17.6%) developed PVR and tractional retinal detachment. The average preoperative ODR in RRD patients who did or did not develop PVR was 0.77 ± 0.15 and 0.72 ± 0.2, respectively (p-value: 0.37). Age, lens status and retinal detachment duration did not correlate with post-operative PVR or tractional retinal detachment in this study cohort.
(View poster)
Conclusions
PVR is a challenging cause of retinal detachment after RRD repair. In this study cohort, pre-operative ODR measurements were not statistically significantly different between patients who developed and did not develop postoperative PVR. The study’s sample size was limited by its strict inclusion criteria and the unnecessity of pre-operative SD-OCT imaging in all RRD patients.
Financial Interests
None to disclose
References
1. Schachat, A. (2018). Ryans Retina. Elsevier.
2. "Proliferative Vitreoretinopathy". Retina and Vitreous of Texas. Retrieved 2009-05-28.
3. Machemer R: Pathogenesis and classification of massive periretinal proliferation. Br J Ophthalmol 1978; 62: pp. 737-747
4. Leaver P. K. (1995). Proliferative vitreoretinopathy. The British journal of ophthalmology, 79(10),
871- 2.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE