Hover to pan and click to magnify. Click again to pan at full screen.
Raisa Ghosh1, Aveek Mukherjee2
1,2- Resident Physicians, Saint Peter's University Hospital, New Brunswick, NJ
Raisa Ghosh1, Aveek Mukherjee2
1,2- Resident Physicians, Saint Peter's University Hospital, New Brunswick, NJ
Saint Peter's University Hospital, New Brunswick, NJ
ABSTRACT:
INTRODUCTION
Direct carotid cavernous fistulas (DCCF) occurs mostly due to trauma or aneurysmal rupture.1 Iatrogenic DCCF formation after endovascular thrombectomy is very rare.1
CASE PRESENTATION
61 year old right handed Caucasian female presented from a rehabilitation center with redness, swelling and excessive tearing of both eyes for ten days. She was currently undergoing rehabilitation for recent embolic stroke (one and a half months back) treated with left middle cerebral artery and terminal internal carotid artery mechanical thrombectomy. Her symptoms were accompanied by visual blurriness and pressure like sensation however there was no pain, fever, itching or upper respiratory tract infection symptoms. She was given topical polymyxin drops at the rehabilitation facility without improvement. Her past medical history included paroxysmal Atrial Fibrillation, pacemaker implantation due to sick sinus syndrome, Non-Hodgkin lymphoma (in remission since eight years).
Eye examination showed bilateral conjunctival erythema, chemosis and proptosis of the left eye. Light reflex, accommodation reflex, extra-ocular movements and visual fields were intact bilaterally. Visual acuity was 20/30 in left and 20/50 in right eye. Fundoscopy exam revealed dilated retinal veins bilaterally. Intra-ocular pressure was 20 mmHg (normal range- 8-21mmHg) bilaterally. Neurological examination revealed right sided hemiparesis, right facial nerve palsy, decreased right sided sensation and brisk deep tendon reflexes on the right side due to the recent stroke. There was no thyromegaly.
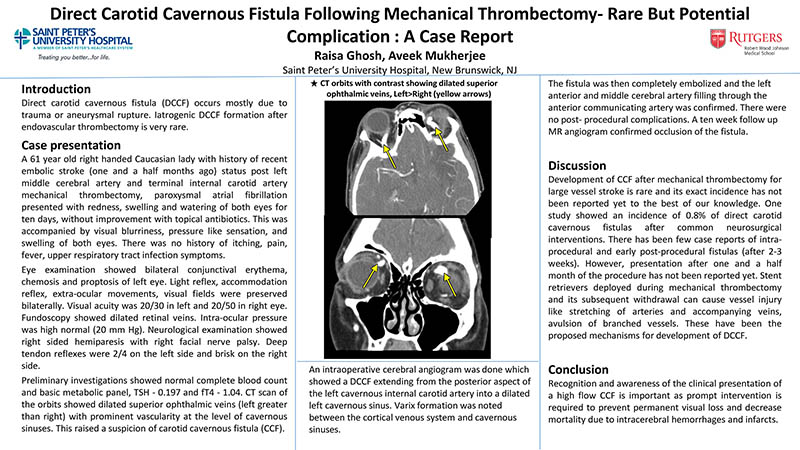
Preliminary investigations showed normal CBC and BMP, decreased TSH- 0.197uIU/ml (0.465-4.68uIU/ml) but normal fT4- 1.04ng/dl (0.61-1.12 ng/dl). CT scan of the orbits showed dilated superior ophthalmic veins (left greater than right) with prominent vascularity at the level of cavernous sinuses. This raised a suspicion of carotid cavernous fistula. A diagnostic cerebral angiogram was done which showed a DCCF extending from the posterior aspect of the left cavernous internal carotid artery into a dilated left cavernous sinus. Varix formation was noted between the cortical venous system and cavernous sinuses. Due to risk of progression and potential complications (Including blindness) the fistula was treated with endovascular embolization. There were no post-procedural complications. Left anterior and middle cerebral artery filling through the anterior communicating artery was confirmed during the procedure and a ten week follow up Magnetic Resonance angiogram confirmed occlusion of the fistula.
Discussion
Development of DCCF after mechanical thrombectomy for large vessel stroke is rare and its exact incidence has not been reported yet2. One study showed an incidence of 0.8% of DCCF after common neurosurgical interventions3. There has been few case reports of intra-procedural and early post-procedural fistulas (after 2-3 weeks)1,4. However, presentation after one and a half month of the procedure has not been reported yet. Stent retrievers deployed during mechanical thrombectomy and its subsequent withdrawal can cause vessel injury like stretching of arteries and accompanying veins, avulsion of branched vessels2.
Conclusion
Recognition and awareness of the clinical presentation of a DCCF is important as prompt intervention is required to prevent permanent visual loss and to decrease mortality due to intracerebral hemorrhages and infarcts especially due to varix formation as in our case1.

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE