Hover to pan and click to magnify. Click again to pan at full screen.
Shah1, Khuttan1, Tobiasson1
1.St. Peters University Hospital, New Brunswick, NJ
Shah1, Khuttan1, Tobiasson1
1.St. Peters University Hospital, New Brunswick, NJ
Saint Peter's University Hospital
ABSTRACT:
A 71-year-old lady with a past medical history of COPD, Hypertension, Hyperlipidemia, Anxiety presented to the emergency department with sudden onset swelling and redness of her left leg since 8 am on the morning of admission. On the day prior to the swelling, the patient was in her usual state of health performing household chores and grocery shopping when she noticed some discomfort in her left posterior thigh which She described as a constant, non-radiating, “twinge”, rated 3/10 in severity. It did not interfere with her daily activities, so she ignored it and went to bed. The next morning, the patient woke up with moderate swelling and redness of her left leg which was more noticeable in her left upper thigh. She was able to ambulate without difficulty. Over the course of the morning, she noticed some blueish discoloration of her left foot. She now suspected that her symptoms were related to poor circulation and began walking a great deal to re-establish blood flow. Despite her efforts, however, the swelling and redness worsened and had now spread to involve the entirety of her left lower extremity. Her left leg was now significantly larger, warmer, and more erythematous than her right. This was the first time she had ever experienced anything like this. Of note, she had a 50 pack-year smoking history.
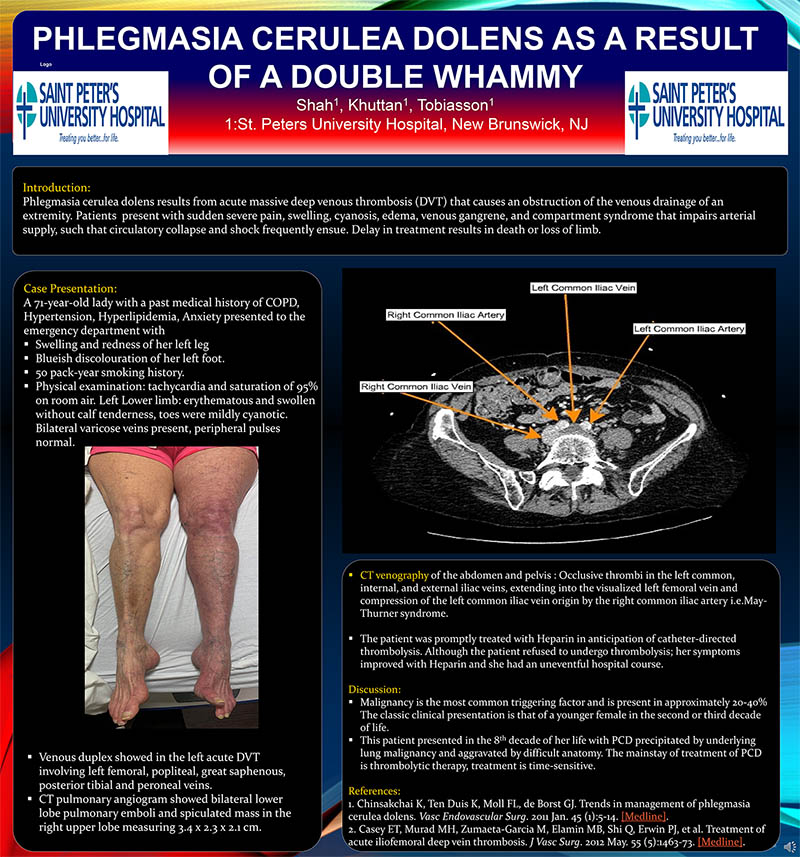
Physical examination was remarkable for tachycardia at 119 and saturation of 95% on room air. The left Lower limb was markedly erythematous and swollen without calf tenderness. Soles of her left foot appeared mildly cyanotic. Bilateral varicose veins present, peripheral pulses normal. Venous duplex showed in the left acute deep vein thrombosis involving left femoral, popliteal s, great saphenous, posterior tibial, and peroneal veins. CT pulmonary angiogram showed bilateral lower lobe pulmonary emboli and spiculated mass in the right upper lobe measuring 3.4 x 2.3 x 2.1 cm. To further investigate the extensive DVT a CT venography of the abdomen and pelvis was done that showed occlusive thrombi in the left common, internal, and external iliac veins, extending into the visualized left femoral vein and compression of the left common iliac vein origin by the right common iliac artery i.e.May-Thurner syndrome. The patient was promptly treated with Heparin in anticipation of catheter-directed thrombolysis. Although the patient refused to undergo thrombolysis; her symptoms improved with Heparin and she had an uneventful hospital course. Malignancy is the most common triggering factor and is present in approximately 20-40% of patients with phlegmasia cerulean dolens (PCD).1The classic clinical presentation is that of a younger female in the second or third decade of life presenting acutely with left lower extremity swelling that involves the entire limb. This patient presented in the 8th decade of her life with PCD precipitated by underlying lung malignancy and aggravated by difficult anatomy. The mainstay of treatment of PCD is thrombolytic therapy2, treatment is time-sensitive

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE