Hover to pan and click to magnify. Click again to pan at full screen.
Dr. Akshay Chaudhari, PGY1, Saint Peter's University Hospital
Dr. Monarch Shah, PGY2, Saint Peter's University Hospital
Dr. Shweta Chaudhary, PGY1, Saint Peter's University Hospital
Dr. Anil Anandam, Attending Physician, Saint Peter's University Hospital
Dr. Akshay Chaudhari, PGY1, Saint Peter's University Hospital
Dr. Monarch Shah, PGY2, Saint Peter's University Hospital
Dr. Shweta Chaudhary, PGY1, Saint Peter's University Hospital
Dr. Anil Anandam, Attending Physician, Saint Peter's University Hospital
Saint Peter's University Hospital
ABSTRACT:
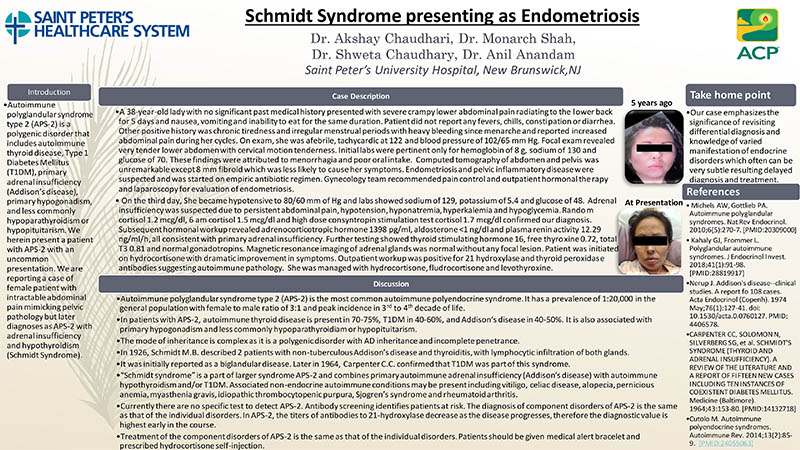
Schmidt Syndrome presenting as Endometriosis
Introduction
Autoimmune polyglandular syndrome type 2 (APS-2) is a polygenic disorder that includes autoimmune thyroid disease, Type 1 Diabetes Mellitus (T1DM), primary adrenal insufficiency (Addison’s disease), primary hypogonadism, and less commonly hypoparathyroidism or hypopituitarism. We herein present a patient with APS-2 with an uncommon presentation. We are reporting a case of female patient with intractable abdominal pain mimicking pelvic pathology but later diagnoses as APS-2 with adrenal insufficiency and hypothyroidism (Schmidt Syndrome).
Case Description
A 38-year-old lady with no significant past medical history presented with severe crampy lower abdominal pain radiating to the lower back for 5 days. The patient also had nausea, vomiting and inability to eat for the same duration. Patient did not report any fevers, chills, constipation or diarrhea. Other positive history was chronic tiredness and irregular menstrual periods with heavy bleeding since menarche and reported increased abdominal pain during her cycles. On exam, she was afebrile, tachycardic at 122 and blood pressure of 102/65 mm mercury. Focal exam revealed very tender lower abdomen with cervical motion tenderness. Initial labs were pertinent only for hemoglobin of 8 grams per deciliter, sodium of 130 and glucose of 70. These findings were attributed to menorrhagia and poor oral intake. Computed tomography of abdomen and pelvis was unremarkable except 8 mm fibroid which was less likely to cause her symptoms. Endometriosis and pelvic inflammatory disease were suspected and was started on empiric antibiotic regimen. Gynecology team recommended pain control and outpatient hormonal therapy and laparoscopy for evaluation of endometriosis. On the third day, She became hypotensive to 80/60 mm of Hg and labs showed sodium of 129, potassium of 5.4 and glucose of 48. Adrenal insufficiency was suspected due to persistent abdominal pain, hypotension, hyponatremia, hyperkalemia and hypoglycemia. Random cortisol 1.2 mcg/dl, 6 am cortisol 1.5 mcg/dl and high dose consyntropin stimulation test cortisol 1.7 mcg/dl confirmed our diagnosis. Subsequent hormonal workup revealed adrenocorticotropic hormone 1398 pg/ml, aldosterone <1 ng/dl and plasma renin activity 12.29 ng/ml/h, all consistent with primary adrenal insufficiency. Further testing showed thyroid stimulating hormone 16, free thyroxine 0.72, total T3 0.81 and normal gonadotropins. Magnetic resonance imaging of adrenal glands was normal without any focal lesion. Patient was initiated on hydrocortisone with dramatic improvement in symptoms. Outpatient workup was positive for 21 hydroxylase and thyroid peroxidase antibodies suggesting autoimmune pathology. Quantiferon gold test was also positive with a normal chest X-ray. She was managed with hydrocortisone, fludrocortisone and levothyroxine.
Discussion
• Autoimmune polyglandular syndrome type 2 (APS-2) is the most common autoimmune polyendocrine syndrome. It has a prevalence of 1:20,000 in the general population with female to male ratio of 3:1 and peak incidence in 3rd to 4th decade of life.
• In patients with APS-2, autoimmune thyroid disease is present in 70-75%, T1DM in 40-60%, and Addison’s disease in 40-50%. It is also associated with primary hypogonadism and less commonly hypoparathyroidiam or hypopituitarism.
• The mode of inheritance is complex as it is a polygenic disorder with AD inheritance and incomplete penetrance.
• In 1926, Schmidt M.B. described 2 patients with non-tuberculous Addison’s disease and thyroiditis, with lymphocytic infiltration of both glands.
• It was initially reported as a biglandular disease. Later in 1964, Carpenter C.C. confirmed that T1DM was part of this syndrome.
• “Schmidt syndrome” is a part of larger syndrome APS-2 and combines primary autoimmune adrenal insufficiency (Addison’s disease) with autoimmune hypothyroidism and/or T1DM. Associated non-endocrine autoimmune conditions may be present including vitiligo, celiac disease, alopecia, pernicious anemia, myasthenia gravis, idiopathic thrombocytopenic purpura, Sjogren’s syndrome and rheumatoid arthritis.
• Currently there are no specific test to detect APS-2. Antibody screening identifies patients at risk. The diagnosis of component disorders of APS-2 is the same as that of the individual disorders. In APS-2, the titers of antibodies to 21-hydroxylase decrease as the disease progresses, therefore the diagnostic value is highest early in the course.
• Treatment of the component disorders of APS-2 is the same as that of the individual disorders. Patients should be given medical alert bracelet and prescribed hydrocortisone self-injection.
Take home point
Our case emphasizes the significance of revisiting differential diagnosis and knowledge of varied manifestation of endocrine disorders which often can be very subtle resulting delayed diagnosis and treatment.

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE