Hover to pan and click to magnify. Click again to pan at full screen.
South Texas Orthopaedic Research Institute, Laredo, Texas 78045, USA; University of The Incarnate Word School of Osteopathic Medicine, San Antonio, Texas 78209, USA; Future Biologics, Lawrenceville, Georgia 30043, USA; BioIntegrate, Lawrenceville, Georgia 30043, USA; Department of Psychology, Illinois Wesleyan University, Bloomington, Illinois 61701, USA; Department of Musculoskeletal Disorders, School of Medicine and Surgery, University if Salerno, Fisciano 84084, Italy; Queen Mary University of London, Barts and the London School of Medicine and Dentistry, Centre for Sports and Exercise Medicine, London, England; Keele University Faculty of Medicine, School of Pharmacy and Bioengineering, Stroke on Trent, England; Laredo Sports Medicine Clinic, Laredo, Texas 78041, USA;
Hugo C. Rodriguez, MBS; Ashim Gupta, PhD, MBA; Ian Stone, BS; Nicola Maffulli, MD; Anish G. Potty, M
South Texas Orthopaedic Research Institute, Laredo, Texas 78045, USA; University of The Incarnate Word School of Osteopathic Medicine, San Antonio, Texas 78209, USA; Future Biologics, Lawrenceville, Georgia 30043, USA; BioIntegrate, Lawrenceville, Georgia 30043, USA; Department of Psychology, Illinois Wesleyan University, Bloomington, Illinois 61701, USA; Department of Musculoskeletal Disorders, School of Medicine and Surgery, University if Salerno, Fisciano 84084, Italy; Queen Mary University of London, Barts and the London School of Medicine and Dentistry, Centre for Sports and Exercise Medicine, London, England; Keele University Faculty of Medicine, School of Pharmacy and Bioengineering, Stroke on Trent, England; Laredo Sports Medicine Clinic, Laredo, Texas 78041, USA;
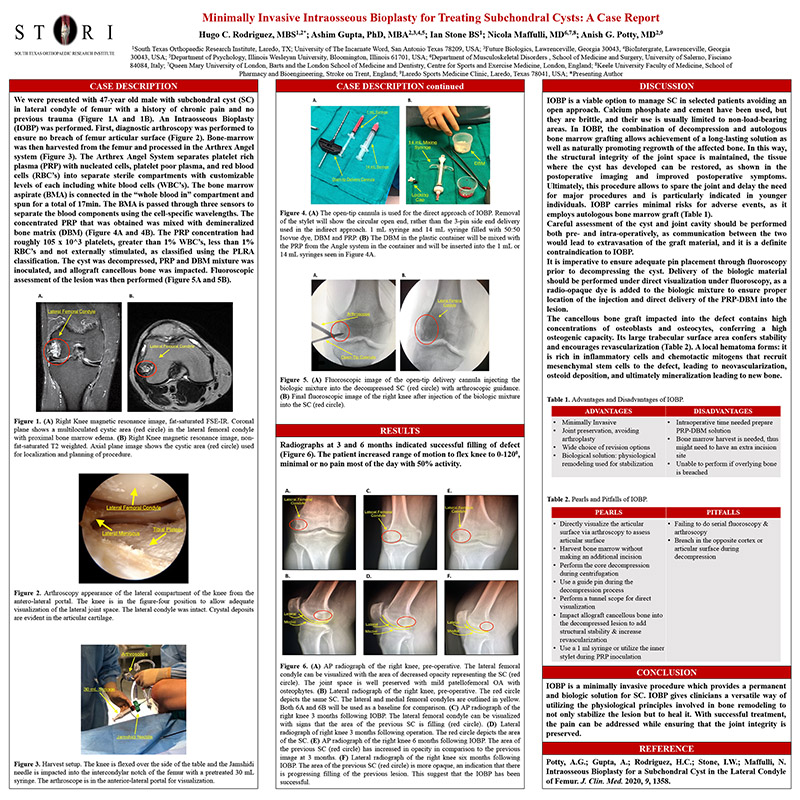
Case Description: We were presented with 47-year old male with subchondral cyst (SC) in lateral condyle of femur with a history of chronic pain and no previous trauma. An Intraosseous Bioplasty (IOBP) was performed. First, diagnostic arthroscopy was performed to ensure no breach of femur articular surface. Bone-marrow was then harvested from the femur and processed in the Arthrex Angel system. The Arthrex Angel System separates platelet rich plasma (PRP) with nucleated cells, platelet poor plasma, and red blood cells (RBC’s) into separate sterile compartments with customizable levels of each including white blood cells (WBC’s). The bone marrow aspirate (BMA) is connected in the “whole blood in” compartment and spun for a total of 17min. The BMA is passed through three sensors to separate the blood components using the cell-specific wavelengths. The concentrated PRP that was obtained was mixed with demineralized bone matrix (DBM). The PRP concentration had roughly 105 x 10^3 platelets, greater than 1% WBC’s, less than 1% RBC’s and not externally stimulated, as classified using the PLRA classification. The cyst was decompressed, PRP and DBM mixture was inoculated, and allograft cancellous bone was impacted. Fluoroscopic assessment of the lesion was then performed.
Assessment/Results: Radiographs at 3 and 6 months indicated successful filling of defect. The patient increased range of motion to flex knee to 0-1200, minimal or no pain most of the day with 50% activity.
Discussion: The combination of decompression and PRP+DBM grafting allowed for maintaining structural integrity of joint space and restoration of affected bone.
Conclusion: IOBP is a minimally invasive procedure which can provide a permanent and biologic solution for SC. IOBP gives clinicians a versatile way of utilizing the physiological principles involved in bone remodeling, where conservative management fails to ameliorate symptoms.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE