Hover to pan and click to magnify. Click again to pan at full screen.
Ian Fong, RN; Julie Chou, RN; Elizabeth Key, RN; et. al.
Ian Fong, RN; Julie Chou, RN; Elizabeth Key, RN; et. al.
UC DAVIS HEALTH - QUALITY IMPROVEMENT, PERIOPERATIVE SERVICES
Background & Purpose
The OR UBPC has been around for more than 5 years,
and is regularly looking to improving its efficacy in order
to better serve the OR as a unit. A well-functioning UBPC
is correlated to improving health across the continuum1
and encouraging nurse engagement in organizational
decision making.2 The success of the UBPC is often
measured by its ability to successfully implement quality
improvement through projects.
Purpose
The purpose of this review is to analyze past project
evaluation data in order to improve the efficacy of project
implementation for future OR UBPC projects. This will
lead to greater nurse-driven improvements to the OR
positively impacting patient care across the continuum.
Design & Methods
A retroactive analysis was conducted utilizing
qualitative project evaluation data collected between
2013 and 2019 in order to determine factors leading to
project success and failure in the Operating Room
UBPC’s history. Specific metrics were identified to track
over the course of every project attempted between
the aforementioned years.
Analysis
Data was collected on all projects between 2013 and
2019 using the following metrics: project success,
barriers to success, reasons for success, meeting
attendance, project members, and total projects per
year.
Results
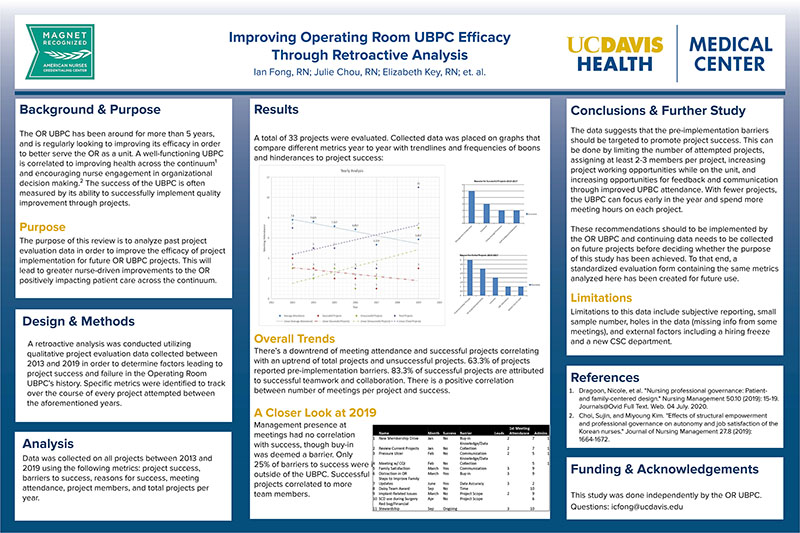
A total of 33 projects were evaluated. Collected data was placed on graphs that
compare different metrics year to year (Image: See poster)
Overall Trends
There’s a downtrend of meeting attendance and successful projects correlating
with an uptrend of total projects and unsuccessful projects. 63.3% of projects
reported pre-implementation barriers. 83.3% of successful projects are attributed
to successful teamwork and collaboration. There is a positive correlation
between number of meetings per project and success.
A Closer Look at 2019
Management presence at
meetings had no correlation
with success, though buy-in
was deemed a barrier. Only
25% of barriers to success were identified as originating
outside of the UBPC. Successful
projects correlated to more
team members. (Image: See poster)
Conclusions & Further Study
The data suggests that the pre-implementation barriers
should be targeted to promote project success. This can
be done by limiting the number of attempted projects,
assigning at least 2-3 members per project, increasing
project working opportunities while on the unit, and
increasing opportunities for feedback and communication
through improved UPBC attendance. With fewer projects,
the UBPC can focus early in the year and spend more
meeting hours on each project.
These recommendations should to be implemented by
the OR UBPC and continuing data needs to be collected
on future projects before deciding whether the purpose
of this study has been achieved. To that end, a
standardized evaluation form containing the same metrics
analyzed here has been created for future use.
Limitations
Limitations to this data include subjective reporting, small
sample number, holes in the data (missing info from some
meetings), and external factors including a hiring freeze
and a new CSC department.
References
1. Dragoon, Nicole, et al. "Nursing professional governance: Patientand
family-centered design." Nursing Management 50.10 (2019): 15-19.
Journals@Ovid Full Text. Web. 04 July. 2020.
2. Choi, Sujin, and Miyoung Kim. "Effects of structural empowerment
and professional governance on autonomy and job satisfaction of the
Korean nurses."
Funding & Acknowledgements
This study was done independently by the OR UBPC.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE