Hover to pan and click to magnify. Click again to pan at full screen.
Jessinnie Ferreras, RN, BSN, CMSRN; Felicidad Loomis, RN, MSN; Eric Moore, RN, BSN, MBA, NEA-BC; Allison Ryan, RN, BSN, CMSRN; Cambria Roberts, RN, BSN, CMSRN; Anthony Splendorio, RN, BSN; Daneva Tabingo, RN, BSN, CMSRN; Rosalyn Taijeron, RN, BSN, CMSRN; Alice Ujiie, RN, BSN, CMSRN
Jessinnie Ferreras, RN, BSN, CMSRN; Felicidad Loomis, RN, MSN; Eric Moore, RN, BSN, MBA, NEA-BC; Allison Ryan, RN, BSN, CMSRN; Cambria Roberts, RN, BSN, CMSRN; Anthony Splendorio, RN, BSN; Daneva Tabingo, RN, BSN, CMSRN; Rosalyn Taijeron, RN, BSN, CMSRN; Alice Ujiie, RN, BSN, CMSRN
UC DAVIS HEALTH - EVIDENCE-BASED PRACTICE
Background
Workplace violence in the hospital leads to patient and staff injury, increased healthcare costs, decreased staff satisfaction, and possibly even decreased staff retention as eluded to in the most recent Staff Engagement Survey results.
Purpose
The aim of this project is to decrease the number of violent encounters on a medical surgical specialty unit through the inclusion of an individualized plan of care that requires coordination with the interdisciplinary team. The safety of the patient as well as the safety of each team member are the focus of the efforts made in implementing this multifaceted and individualized plan of care.
PICO Question
Will the number of violent encounters decrease on an acute care unit if an individualized behavioral management plan is implemented with a patient who has a history of violent episodes, and continues to be an elevated risk for violence?
Design & Methods
Staff were educated on the expectations for working directly with a known violent patient and trained on how to participate in Planned Potentially Violent Encounters (PPVE) through classes, mandatory annual trainings, and by directly participating in PPVEs on the unit. The following interventions and best practices were utilized in the daily workflow:
• Change of shift huddle – The charge nurse from the previous shift discusses violence and potentially violent behavior during change of shift huddle.
• Change of shift bedside report – Bedside report is conducted as a team including the charge nurses and the shift nurses for patient with known violent behaviors.
• Planned Potentially Violent Encounters (PPVE) – A protocol used for patients with an “elevated risk for violence” as evidenced by a history of violent behavior.
• Interprofessional huddle – Mental health huddles are conducted on a regular basis and may include members from the Lift team, psychiatric NP, patient’s primary doctor, private safety officers (PSO), Davis Police Department (DPD), nursing supervisor, charge nurse, shift nurse, and/or unit manager. The goal of the huddle is to increase safety and consistent patient care. Significant changes in the plan of care are made in collaboration with the team.
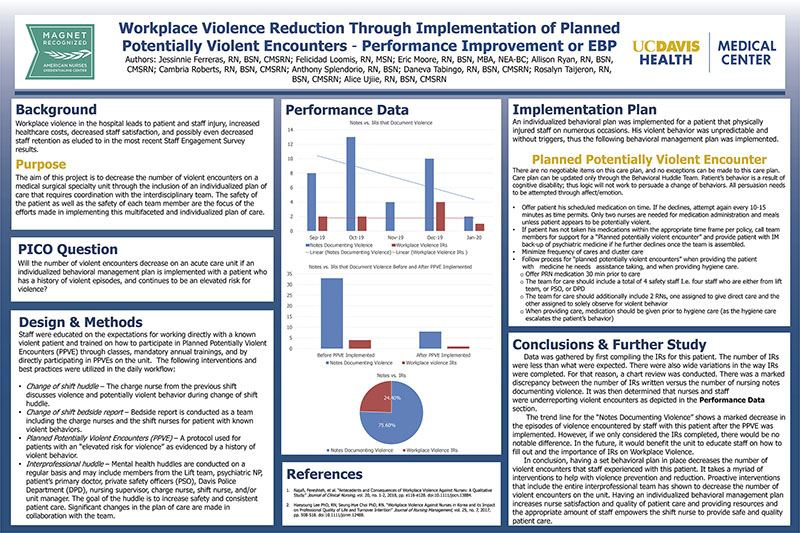
Performance Data
(see poster)
Implementation Plan
An individualized behavioral plan was implemented for a patient that physically injured staff on numerous occasions. His violent behavior was unpredictable and without triggers, thus the following behavioral management plan was implemented.
Planned Potentially Violent Encounter
There are no negotiable items on this care plan, and no exceptions can be made to this care plan. Care plan can be updated only through the Behavioral Huddle Team. Patient’s behavior is a result of cognitive disability; thus logic will not work to persuade a change of behaviors. All persuasion needs to be attempted through affect/emotion.
• Offer patient his scheduled medication on time. If he declines, attempt again every 10-15 minutes as time permits. Only two nurses are needed for medication administration and meals unless patient appears to be potentially violent.
• If patient has not taken his medications within the appropriate time frame per policy, call team members for support for a “Planned potentially violent encounter” and provide patient with IM back-up of psychiatric medicine if he further declines once the team is assembled.
• Minimize frequency of cares and cluster care
Follow process for “planned potentially violent encounters” when providing the patient with medicine he needs assistance taking, and when providing hygiene care.
• Offer PRN medication 30 min prior to care
• The team for care should include a total of 4 safety staff I.e. four staff who are either from lift team, or PSO, or DPD
• The team for care should additionally include 2 RNs, one assigned to give direct care and the other assigned to solely observe for violent behavior
• When providing care, medication should be given prior to hygiene care (as the hygiene care escalates the patient’s behavior)
Conclusions & Further Study
Data was gathered by first compiling the IRs for this patient. The number of IRs were less than what were expected. There were also wide variations in the way IRs were completed. For that reason, a chart review was conducted. There was a marked discrepancy between the number of IRs written versus the number of nursing notes documenting violence. It was then determined that nurses and staff were underreporting violent encounters as depicted in the Performance Data section.
The trend line for the “Notes Documenting Violence” shows a marked decrease in the episodes of violence encountered by staff with this patient after the PPVE was implemented. However, if we only considered the IRs completed, there would be no notable difference. In the future, it would benefit the unit to educate staff on how to fill out and the importance of IRs on Workplace Violence.
In conclusion, having a set behavioral plan in place decreases the number of violent encounters that staff experienced with this patient. It takes a myriad of interventions to help with violence prevention and reduction. Proactive interventions that include the entire interprofessional team has shown to decrease the number of violent encounters on the unit. Having an individualized behavioral management plan increases nurse satisfaction and quality of patient care and providing resources and the appropriate amount of staff empowers the shift nurse to provide safe and quality patient care.
References
1. Najafi, Fereshteh, et al. “Antecedents and Consequences of Workplace Violence Against Nurses: A Qualitative Study.” Journal of Clinical Nursing, vol. 20, no. 1-2, 2018, pp. e116-e128. doi:10.1111/jocn.13884.
2. Haeyoung Lee PhD, RN, Seung-Hye Choi PhD, RN. “Workplace Violence Against Nurses in Korea and its Impact on Professional Quality of Life and Turnover Intention” Journal of Nursing Management, vol. 25, no. 7, 2017, pp. 508-518. doi:10.1111/jonm.12488.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE