Hover to pan and click to magnify. Click again to pan at full screen.
Charity Bigornia, RN, BSN, CCRN, UBPC chair; Erica Miller, RN, BSN, CCRN, UBPC co-chair; Cherie Noll, RN, BSN; Korinn Wiest, RN, BSN, CCRN; Melissa Davis, RN, MSN, CCRN; Katherine Jordan, RN, MSN, CCRN; Myra Tabaldo, RN, MSN, CCRN; Connie Ngo, RN, BSN, CCRN; Justin Massaro, RN, BSN; Deann Hayes, RN, MSN, SICU Manager; Farrah Reynoso, RN, BSN, Quality and Safety Champion; Victoria Smith, MSN, RN, CNL, CCRN, Quality & Safety Champion
Charity Bigornia, RN, BSN, CCRN, UBPC chair; Erica Miller, RN, BSN, CCRN, UBPC co-chair; Cherie Noll, RN, BSN; Korinn Wiest, RN, BSN, CCRN; Melissa Davis, RN, MSN, CCRN; Katherine Jordan, RN, MSN, CCRN; Myra Tabaldo, RN, MSN, CCRN; Connie Ngo, RN, BSN, CCRN; Justin Massaro, RN, BSN; Deann Hayes, RN, MSN, SICU Manager; Farrah Reynoso, RN, BSN, Quality and Safety Champion; Victoria Smith, MSN, RN, CNL, CCRN, Quality & Safety Champion
UC DAVIS HEALTH - QUALITY IMPROVEMENT
BACKGROUND
Central Line Associated Blood Stream Infection (CLABSI) rates in the Surgical Intensive Care Unit (SICU) continue to fluctuate despite hospital wide initiatives. An audit of SICU nursing practice showed a knowledge deficit in central venous catheter (CVC)and intravenous (IV)line management.
A unit-based project was created to:
1. Increase compliance with hospital policies.
2. Reduce SICU CLABSI rates.
The project consisted of three parts:
• Instituting two-person dressing change.
• Providing education on proper maintenance of CVCs.
• Eliminating designated line change nights.
PURPOSE
The purpose of this project was to decrease the CLABSI rate to be below the National Database of Nursing Quality (NDNQI) mean by modifying nursing practice in caring for IVs/CVCs.
(see poster)
METHODS
In August and September 2019, data was obtained regarding staff compliance with current vascular access management policies, knowledge deficits regarding proper practice were identified, and an education plan was developed to address those areas.
The changes in practice and the new expectations were communicated to staff via:
• Shift huddle
• Formal education entitled “Line Maintenance for HAI Reduction,” was completed during the August staff meeting, mandatory SICU September Skills Day, and individual/small group education in SICU by two of the UBPC members
• Handouts were provided during skills day, posted in the unit on the UBPC board and placed in each patient room (see Figure to right)
Observation and chart auditing were completed to assess nurses’ compliance with the new changes.
Data was collected in December 2019, three months after practice change implementation.
RESULTS/FINDINGS
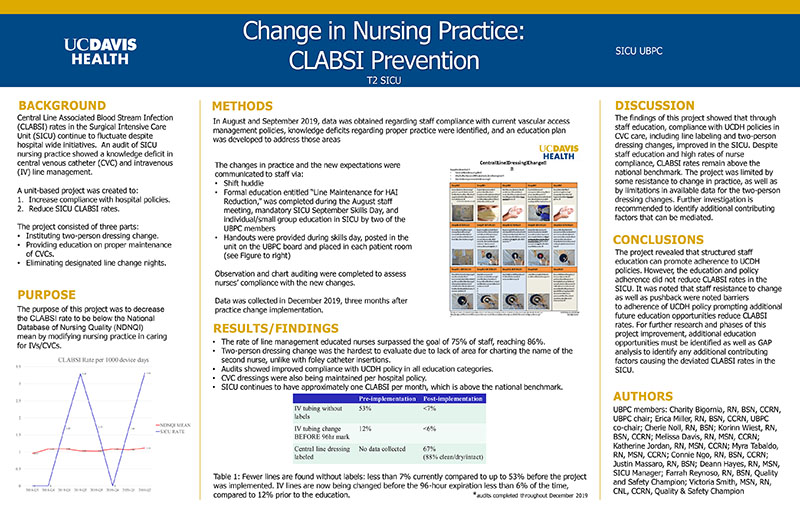
• The rate of line management educated nurses surpassed the goal of 75% of staff, reaching 86%.
• Two-person dressing change was the hardest to evaluate due to lack of area for charting the name of the second nurse, unlike with foley catheter insertions.
• Audits showed improved compliance with UCDH policy in all education categories.
• CVC dressingswere also being maintained per hospital policy.
• SICU continues to have approximately one CLABSI per month, which is above the national benchmark.
(see poster)
Table 1: Fewer lines are found without labels: less than 7% currently compared to up to 53% before the project was implemented. IV lines are now being changed before the 96-hour expiration less than 6% of the time, compared to 12% prior to the education.
*audits completed throughout December 2019
DISCUSSION
The findings of this project showed that through staff education, compliance with UCDH policies in CVC care, including line labeling and two-person dressing changes, improved in the SICU. Despite staff education and high rates of nurse compliance, CLABSI rates remain above the national benchmark. The project was limited by some resistance to change in practice, as well as by limitations in available data for the two-person dressing changes. Further investigation is recommended to identify additional contributing factors that can be mediated.
CONCLUSIONS
The project revealed that structured staff education can promote adherence to UCDH policies. However, the education and policy adherence did not reduce CLABSI rates in the SICU. It was noted that staff resistance to change as well as pushback were noted barriers
to adherence of UCDH policy prompting additional future education opportunities reduce CLABSI rates. For further research and phases of this project improvement, additional education opportunities must be identified as well as GAP analysis to identify any additional contributing factors causing the deviated CLABSI rates in the SICU.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE