Hover to pan and click to magnify. Click again to pan at full screen.
Brenda Inman, MSN, RNC-OB, C-EFM and Julie Janke, BSN, RN
Brenda Inman, MSN, RNC-OB, C-EFM and Julie Janke, BSN, RN
UC DAVIS HEALTH - EVIDENCE-BASED PRACTICE
Background
A new hospital protocol was developed for administration of brexanolone in collaboration with nursing, obstetrics, anesthesia, pharmacy, and administration. Under the protocol, the patient was placed in 1:1 nursing care throughout her admission. The patient’s vital signs and level of sedation were closely monitored because excessive sedation was the primary risk noted in clinical trials. The UC Davis Health protocol incorporated continuous pulse ox and ETCO2 monitoring. Brexanolone is an intravenous medication newly approved by the FDA for the treatment of postpartum depression. Brexanolone moderates receptor sites in the brain because hormone levels rise during pregnancy and decline sharply during the postpartum period. The infusion lasts 60 hours with different infusion rates titrated throughout the administration. Each bag of the medication is stable at room temperature for 12 hours once reconstituted.
A G4P2 with a history of postpartum depression (PPD) and posttraumatic stress disorder (PTSD) was the first patient on the west coast to receive an infusion of brexanolone therapy under hospital protocol after the completion of clinical trials. The patient was selected after a careful screening process. The patient received the infusion approximately 2 months after the delivery of her second child. The patient had tried other oral medications for the treatment of PPD and PTSD without success.
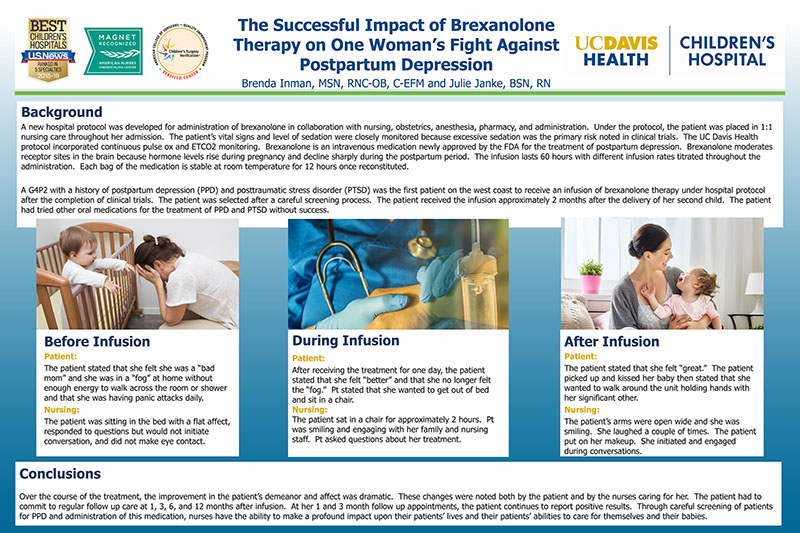
Before Infusion
Patient:
The patient stated that she felt she was a “bad mom” and she was in a “fog” at home without enough energy to walk across the room or shower and that she was having panic attacks daily.
Nursing:
The patient was sitting in the bed with a flat affect, responded to questions but would not initiate conversation, and did not make eye contact.
During Infusion
Patient:
After receiving the treatment for one day, the patient stated that she felt “better” and that she no longer felt the “fog.” Pt stated that she wanted to get out of bed and sit in a chair.
Nursing:
The patient sat in a chair for approximately 2 hours. Pt was smiling and engaging with her family and nursing staff. Pt asked questions about her treatment.
After Infusion
Patient:
The patient stated that she felt “great.” The patient picked up and kissed her baby then stated that she wanted to walk around the unit holding hands with her significant other.
Nursing:
The patient’s arms were open wide and she was smiling. She laughed a couple of times. The patient put on her makeup. She initiated and engaged during conversations.
Conclusions
Over the course of the treatment, the improvement in the patient’s demeanor and affect was dramatic. These changes were noted both by the patient and by the nurses caring for her. The patient had to commit to regular follow up care at 1, 3, 6, and 12 months after infusion. At her 1 and 3 month follow up appointments, the patient continues to report positive results. Through careful screening of patients for PPD and administration of this medication, nurses have the ability to make a profound impact upon their patients’ lives and their patients’ abilities to care for themselves and their babies.
Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
