Hover to pan and click to magnify. Click again to pan at full screen.
UC DAVIS CHILDREN’S HOSPITAL
Michelle Linenberger MSN Ed, RN, CCRN-K, NPD-BC
Michelle Linenberger MSN Ed, RN, CCRN-K, NPD-BC
UC DAVIS CHILDREN’S HOSPITAL - Quality Improvement
Background
• The only nationally ranked comprehensive Children’s Hospital (within an adult hospital) in Sacramento serving 33 counties, covering 65,000 square miles, with nearly 8000 pediatric admissions per year.
• The Central Valley’s only level 1 pediatric trauma center and the West Coast’s first and California’s only level I children’s surgery center as verified by the American College of Surgeons.
• The complex issue of caring for a patient at the end of life in the pediatric intensive care unit is one that nurses are often not prepared for. Education is often focused on caring for a specific population and diagnosis or simulation training for resuscitative efforts. Pediatric Intensive Care Unit (PICU) nurses witness a tremendous amount of human suffering at the end of life and often receive little to no training to provide competent and compassionate care at the end of life.
Purpose
Purpose of this project was to develop an educational opportunity to improve the care of pediatric patients and families at the end of life in the PICU by providing an active learning environment with simulation education. The population of nurses that this education was targeted for were newly hired nurses to the PICU. This group of newly hired nurses ranged in experience level from new graduate nurses to 18 years of nursing experience.
Professional Practice Gap
• A needs assessment was conducted to determine the knowledge and skills needed to care for this patient population. Data collection methods included focus groups as well as the dissemination of a survey. From these findings a gap analysis was identified along with the development of target goals.
• The annual children’s hospital education survey showed that 82% of the nurses wanted more education on end of life care to feel prepared to care for not only their patients, but their families as well.
Implementation
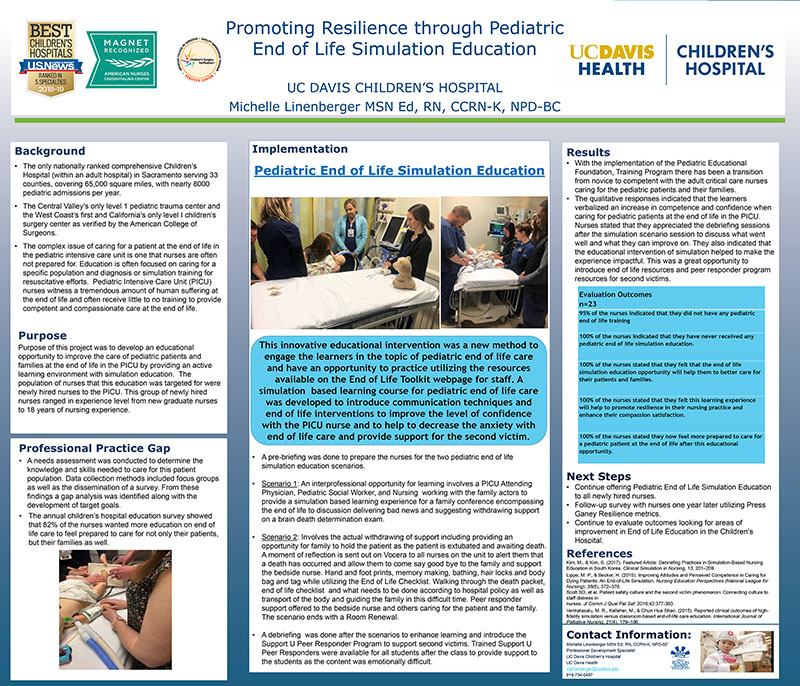
Pediatric End of Life Simulation Education
This innovative educational intervention was a new method to engage the learners in the topic of pediatric end of life care and have an opportunity to practice utilizing the resources available on the End of Life Toolkit webpage for staff. A simulation based learning course for pediatric end of life care was developed to introduce communication techniques and end of life interventions to improve the level of confidence with the PICU nurse and to help to decrease the anxiety with end of life care and provide support for the second victim.
• A pre-briefing was done to prepare the nurses for the two pediatric end of life simulation education scenarios.
• Scenario 1: An interprofessional opportunity for learning involves a PICU Attending Physician, Pediatric Social Worker, and Nursing working with the family actors to provide a simulation based learning experience for a family conference encompassing the end of life to discussion delivering bad news and suggesting withdrawing support on a brain death determination exam.
• Scenario 2: Involves the actual withdrawing of support including providing an opportunity for family to hold the patient as the patient is extubated and awaiting death. A moment of reflection is sent out on Vocera to all nurses on the unit to alert them that a death has occurred and allow them to come say good bye to the family and support the bedside nurse. Hand and foot prints, memory making, bathing, hair locks and body bag and tag while utilizing the End of Life Checklist. Walking through the death packet, end of life checklist and what needs to be done according to hospital policy as well as transport of the body and guiding the family in this difficult time. Peer responder support offered to the bedside nurse and others caring for the patient and the family. The scenario ends with a Room Renewal.
• A debriefing was done after the scenarios to enhance learning and introduce the Support U Peer Responder Program to support second victims. Trained Support U Peer Responders were available for all students after the
Results
• With the implementation of the Pediatric Educational Foundation, Training Program there has been a transition from novice to competent with the adult critical care nurses caring for the pediatric patients and their families.
• The qualitative responses indicated that the learners verbalized an increase in competence and confidence when caring for pediatric patients at the end of life in the PICU. Nurses stated that they appreciated the debriefing sessions after the simulation scenario session to discuss what went well and what they can improve on. They also indicated that the educational intervention of simulation helped to make the experience impactful. This was a great opportunity to introduce end of life resources and peer responder program resources for second victims.
Next Steps
• Continue offering Pediatric End of Life Simulation Education to all newly hired nurses.
• Follow-up survey with nurses one year later utilizing Press Ganey Resilience metrics.
• Continue to evaluate outcomes looking for areas of improvement in End of Life Education in the Children’s Hospital.
References
Kim, M., & Kim, S. (2017). Featured Article: Debriefing Practices in Simulation-Based Nursing Education in South Korea. Clinical Simulation in Nursing, 13, 201–209.
Lippe, M. P., & Becker, H. (2015). Improving Attitudes and Perceived Competence in Caring for Dying Patients: An End-of-Life Simulation. Nursing Education Perspectives (National League for Nursing), 36(6), 372–378.
Scott SD, et al. Patient safety culture and the second victim phenomenon: Connecting culture to staff distress in nurses. Jt Comm J Qual Pat Saf. 2016;42:377-383.
Venkatasalu, M. R., Kelleher, M., & Chun Hua Shao. (2015). Reported clinical outcomes of highfidelity simulation versus classroom-based end-of-life care education. International Journal of Palliative Nursing, 21(4), 179–186.

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE