Hover to pan and click to magnify. Click again to pan at full screen.
Trauma Nursing Unit (Davis 11) Unit Based Practice Council
Rebecca Dutra/Michael Galinato
Rebecca Dutra/Michael Galinato - Trauma Nursing Unit (Davis 11) Unit Based Practice Council
UC DAVIS HEALTH - QUALITY IMPROVEMENT - BEST PEOPLE & PRACTICE ENVIRONMENT - NURSING - TRAUMA
Background
The abrupt nature of the mechanism of illness/injury and the varied associated psychosocial issues of patients who are admitted to the Trauma Nursing Unit (TNU) can make the already complex acute care nursing environment exponentially more challenging. TNU nurses often experience workplace violence, emotional and ethical challenges, high acuity, long hours, and fluctuating delivery systems and resources. This impacts overall job satisfaction for nurses as they attempt to keep pace and provide detailed care for patients and their families. In this turbulent space, distress progresses as nurses also struggle to meet educational, licensing, safety measures, family and personal obligations, and the challenge of finding time to provide self-care. Despite growing evidence that adverse events can have dire emotional consequences on health care providers, most clinicians do not receive adequate emotional support (Pratt et al., 2012, p. 35). A reason that health care organizations do not routinely offer emotional support might be that their leaders do not know how to develop and successfully implement a support system (Pratt et al., 2012, p. 35).
Purpose
The TNU nurses aimed to decrease the impact of unit challenges on staff by creating a supportive practice environment that fosters a commitment to collegiality, recognition, and self
Design & Methods
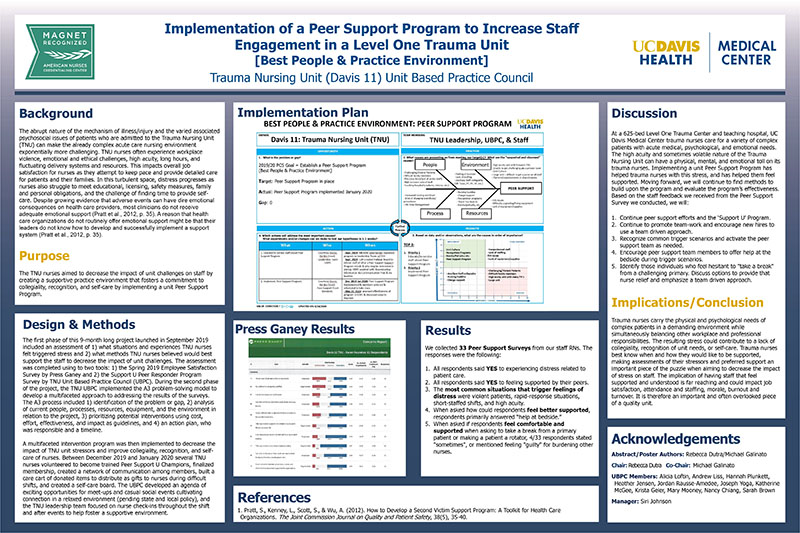
The first phase of this 9-month long project launched in September 2019 included an assessment of 1) what situations and experiences TNU nurses felt triggered stress and 2) what methods TNU nurses believed would best support the staff to decrease the impact of unit challenges. The assessment was completed using to two tools: 1) the Spring 2019 Employee Satisfaction Survey by Press Ganey and 2) the Support U Peer Responder Program Survey by TNU Unit Based Practice Council (UBPC). During the second phase of the project, the TNU UBPC implemented the A3 problem-solving model to develop a multifaceted approach to addressing the results of the surveys. The A3 process included 1) identification of the problem or gap, 2) analysis of current people, processes, resources, equipment, and the environment in relation to the project, 3) prioritizing potential interventions using cost, effort, effectiveness, and impact as guidelines, and 4) an action plan, who was responsible and a timeline.
A multifaceted intervention program was then implemented to decrease the impact of TNU unit stressors and improve collegiality, recognition, and self-care of nurses. Between December 2019 and January 2020 several TNU nurses volunteered to become trained Peer Support U Champions, finalized membership, created a network of communication among members, built a care cart of donated items to distribute as gifts to nurses during difficult shifts, and created a self-care board. The UBPC developed an agenda of exciting opportunities for meet-ups and casual social events cultivating connection in a relaxed environment (pending state and local policy),and the TNU leadership team focused on nurse check-ins throughout the shift and after events to help foster a supportive environment.
Implementation Plan (see poster)
Press Ganey Results (see poster)
Results
We collected 33Peer SupportSurveys from our staff RNs.The responses were the following:
1.All respondents said YESto experiencing distress related to patient care.
2.All respondents said YESto feeling supported by their peers.
3.The most common situations that trigger feelings of distress wereviolent patients, rapid-response situations, short-staffed shifts, and high acuity.
4.When asked how could respondents feel better supported, respondents primarily answered “help at bedside.”
5.When asked if respondents feel comfortable and supported when asking to take a break from a primary patient or making a patient a rotator, 4/33 respondentsstated "sometimes",or mentioned feeling "guilty" for burdening other nurses.
Discussion
At a 625-bed Level One Trauma Center and teaching hospital, UC Davis Medical Center trauma nurses care for a variety of complex patients with acute medical, psychological, and emotional needs. The high acuity and sometimes volatile nature of the Trauma Nursing Unit can have a physical, mental, and emotional toll on its trauma nurses. Implementing a unit Peer Support Program has helped trauma nurses with this stress, and has helped them feel supported. Moving forward, we will continue to find methods to build upon the program and evaluate the program’s effectiveness. Based on the staff feedback we received from the Peer Support Survey we conducted, we will:
1.Continue peer support efforts and the ‘Support U’ Program.
2.Continue to promote team-work and encourage new hires to use a team driven approach.
3.Recognize common trigger scenarios andactivate the peer support team as needed.
4.Encourage peer support team members to offer help at the bedside during trigger scenarios.
5.Identify those individuals who feel hesitant to "take a break" from a challenging primary. Discuss options to provide that nurse relief and emphasize a team driven approach.
Implications/Conclusion
Trauma nurses carry the physical and psychological needs of complex patients in a demanding environment while simultaneously balancing other workplace and professional responsibilities. The resulting stress could contribute to a lack of collegiality, recognition of unit needs, or self-care. Trauma nurses best know when and how they would like to be supported, making assessments of their stressors and preferred support an important piece of the puzzle when aiming to decrease the impact of stress on staff. The implication of having staff that feel supported and understood is far reaching and could impact job satisfaction, attendance and staffing, morale, burnout and turnover. It is therefore an important and often overlooked piece of a quality unit.
References
1. Pratt, S., Kenney, L., Scott, S., & Wu, A. (2012). How to Develop a Second Victim Support Program: A Toolkit for Health Care Organizations. The Joint Commission Journal on Quality and Patient Safety, 38(5), 35-40.
Acknowledgements
Abstract/Poster Authors: Rebecca Dutra/Michael Galinato
Chair: Rebecca Dutra Co-Chair: Michael Galinato
UBPC Members: Alicia Loftin, Andrew Liss, Hannah Plunkett, Heather Jensen, Jordan Rausse-Amedee, Joseph Yoga, Katherine McGee, Krista Geier, Mary Mooney, Nancy Chiang, Sarah Brown
Manager: Siri Johnson

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE