Hover to pan and click to magnify. Click again to pan at full screen.
Karen Semkiw, MPA, RN-C, NEA-BC, CPHQ
Karen Semkiw, MPA, RN-C, NEA-BC, CPHQ
UC DAVIS HEALTH - QUALITY IMPROVEMENT
Introduction
Clinician hand-off is critical in improving communication and preventing significant patient safety events. In 2017, the Joint Commission established Hand-off Communication as a National Patient Safety Goal. While it sounds simple, a high-quality hand-off is complex. In Mid-2018, despite previous attempts at formalizing hand-offs to improve communication, there were some problematic handoffs between the ICUs and the Operating Room that resulted in adverse events, one of which was an ICU patient being left in a hallway. To prevent the recurrence of similar adverse events, we formed a cross-functional process improvement team. This team included nurses from NICU, PICU, OR, and PACU, along with intensivists, surgeons, and anesthesiologists. Our goal was to reduce the number of adverse events without increasing OR turn-over time or causing any other OR delays. After 5 months of weekly meetings, we successfully addressed some serious concerns regarding the transfer of pediatric patients to and from the Children’s Surgery Center by standardizing ICU workflows.
Methods
The team followed the “structured problem solving” system adapted for use at our facility which consists of four elements:
1) Problem definition
•Created a statement describing the issue
•Set goals for the project
•Established measurement for process improvement
2)Analysis
•Developed a process map depicting current state and barriers
•Performed root cause analyses (RCAs) on most serious barriers
3)Prioritization
•Brainstormed possible solutions to issues identified during the RCAs
•Scored possible solutions based on anticipated benefits versus effort to produce
4)Action
•Drafted a plan to deploy highest-scoring interventions
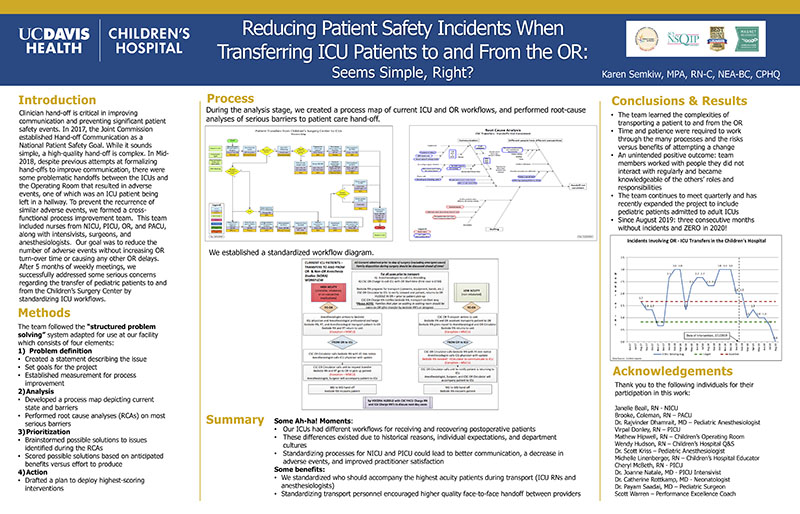
Process
During the analysis stage, we created a process map of current ICU and OR workflows, and performed root-cause analyses of serious barriers to patient care hand-off. (see poster)
Summary
Some Ah-ha! Moments:
Our ICUs had different workflows for receiving and recovering postoperative patients
These differences existed due to historical reasons, individual expectations, and department cultures
Standardizing processes for NICU and PICU could lead to better communication, a decrease in adverse events, and improved practitioner satisfaction
Some benefits:
•We standardized who should accompany the highest acuity patients during transport (ICU RNs and anesthesiologists)
•Standardizing transport personnel encouraged higher quality face-to-face handoff between providers
Conclusions & Results
The team learned the complexities of transporting a patient to and from the OR
•Time and patience were required to work through the many processes and the risks versus benefits of attempting a change
•An unintended positive outcome: team members worked with people they did not interact with regularly and became knowledgeable of the others’ roles and responsibilities
•The team continues to meet quarterly and has recently expanded the project to include pediatric patients admitted to adult ICUs
•Since August 2019: three consecutive months without incidents and ZERO in 2020! (see poster)
Acknowledgements
Thank you to the following individuals for their participation in this work:
Janelle Beall, RN -NICU
Brooke, Coleman, RN –PACU
Dr. Rajvinder Dhamrait, MD –Pediatric Anesthesiologist
Virpal Donley, RN –PICU
Mathew Hipwell, RN –Children’s Operating Room
Wendy Hudson, RN –Children’s Hospital Q&S
Dr. Scott Kriss –Pediatric Anesthesiologist
Michelle Linenberger, RN –Children’s Hospital Educator
Cheryl McBeth, RN -PICU
Dr. Joanne Natale, MD -PICU Intensivist
Dr. Catherine Rottkamp, MD -Neonatologist
Dr. Payam Saadai, MD –Pediatric Surgeon
Scott Warren –Performance Excellence Coach

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE