Hover to pan and click to magnify. Click again to pan at full screen.
Sunitha Sunkara
Sunitha Sunkara
UC DAVIS HEALTH -QUALITY IMPROVEMENT
Background
Central line associated blood stream infections (CLABSIs) lead to prolonged hospital stays, increased health care costs, and increased mortality. Oncology and Bone Marrow Transplant patients are particularly vulnerable to developing CLABSIs due to disease or treatment related neutropenia and due to frequent need for central line access.
Purpose
The aim of this project was to achieve 8 or less CLABSIs for fiscal year 2020. Davis 8, our 35 bed Oncology and Bone Marrow Transplant unit had not been meeting the benchmark minimum performance for 5 out of 8 quarters. For fiscal year 2018, Davis 8 experienced a total of 10 CLABSIs, meeting the benchmark only 3 out of the 8 quarters.
Design & Methods
Our UBPC used an A3 framework to assess what was keeping us from meeting CLABSI benchmarks. We identified three areas of focus: 1) standardized central line dressing changes, 2) re-education on "scrubbing the hub," and 3) increasing the rate of patient CHG bathing.
Our methods included measuring CLABSI rates reported by hospital wide quality and safety champions. Quality and safety champions reported back to Davis 8 UBPC every month if any new CLABSIs resulted and provided RCAs for review.
The patient population included adult patients on Davis 8, primarily composed of the Hematology Oncology and Bone Marrow Transplant services.
Implementation/Plan
Standardized Dressing Technique
September 2019: A centralized dressing change cart was created in the clean utility room containing all supplies necessary for a dressing change, along with new laminated Job-Aides to be used at the bedside during dressing changes. PICC RNs demonstrated proper technique at skills day.
Scrub the Hub
January 2020: At our unit's skills day, we had an interactive activity using black nights and "Glo-Germ" to reinforce proper technique for scrubbing the hub with Prevantix swabs vs regular alcohol swabs.
CHG Bathing
January 2020: In coordination with the infection control team, Davis 8 UBPC implemented laminated CHG bathing signage to display in patient rooms.
PICC Team Involvement
February 2020: PICC nurses began rounding five days a week to assist with 2-RN dressing changes of all central lines. Any dressing found to be compromised (eg. peeling edges or taped down) was to be changed immediately. As bedside RNs became comfortable with proper dressing change technique the PICC Team decreased the frequency of their rounding.
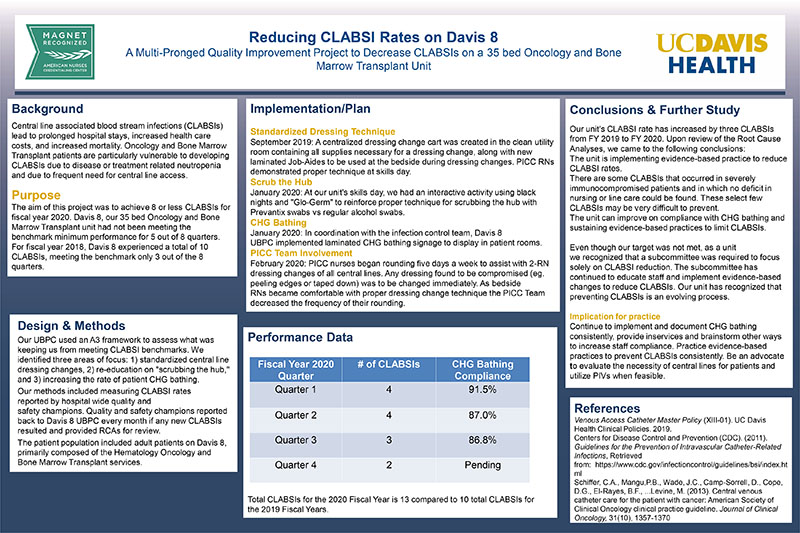
Performance Data (see poster)
Conclusions & Further Study
Our unit's CLABSI rate has increased by three CLABSIs from FY 2019 to FY 2020. Upon review of the Root Cause Analyses, we came to the following conclusions:
The unit is implementing evidence-based practice to reduce CLABSI rates.
There are some CLABSIs that occurred in severely immunocompromised patients and in which no deficit in nursing or line care could be found. These select few CLABSIs may be very difficult to prevent.
The unit can improve on compliance with CHG bathing and sustaining evidence-based practices to limit CLABSIs.
Even though our target was not met, as a unit
we recognized that a subcommittee was required to focus solely on CLABSI reduction. The subcommittee has continued to educate staff and implement evidence-based changes to reduce CLABSIs. Our unit has recognized that preventing CLABSIs is an evolving process.
Implication for practice
Continue to implement and document CHG bathing consistently, provide inservices and brainstorm other ways to increase staff compliance. Practice evidence-based practices to prevent CLABSIs consistently. Be an advocate to evaluate the necessity of central lines for patients and utilize PIVs when feasible.
References
Venous Access Catheter Master Policy (XIII-01). UC Davis Health Clinical Policies. 2019.
Centers for Disease Control and Prevention (CDC). (2011). Guidelines for the Prevention of Intravascular Catheter-Related Infections, Retrieved from: https://www.cdc.gov/infectioncontrol/guidelines/bsi/index.html
Schiffer, C.A., Mangu,P.B., Wade, J.C., Camp-Sorrell, D., Cope, D.G., El-Rayes, B.F., ...Levine, M. (2013). Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. Journal of Clinical Oncology, 31(10), 1357-1370

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE