Hover to pan and click to magnify. Click again to pan at full screen.
Liz North RN, BSN, CCRN, Dawn Harbour MSN, ACCNS-P, CCRN,
Elizabeth Partridge, MD, MPH and Heather Siefkes, MD, MSCI
Liz North RN, BSN, CCRN, Dawn Harbour MSN, ACCNS-P, CCRN, Elizabeth Partridge, MD, MPH and Heather Siefkes, MD, MSCI
UC DAVIS HEALTH -EVIDENCE-BASED PRACTICE
Background
Central line-associated bloodstream infections (CLABSI)
• Major source of hospital-acquired infection (HAI) in the pediatric intensive care unit (PICU)
• Associated with increased morbidity, mortality, and health care costs
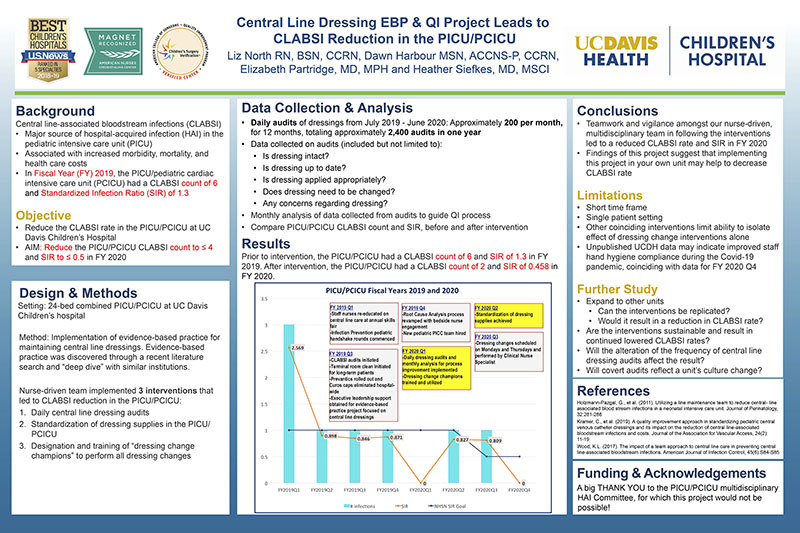
• In Fiscal Year (FY) 2019, the PICU/pediatric cardiac intensive care unit (PCICU) had a CLABSI count of 6 and Standardized Infection Ratio (SIR) of 1.3
Objective
• Reduce the CLABSI rate in the PICU/PCICU at UC Davis Children’s Hospital
• AIM: Reduce the PICU/PCICU CLABSI count to ≤ 4 and SIR to ≤ 0.5 in FY 2020
Design & Methods
Setting: 24-bed combined PICU/PCICU at UC Davis Children’s hospital
Method: Implementation of evidence-based practice for maintaining central line dressings. Evidence-based practice was discovered through a recent literature search and “deep dive” with similar institutions.
Nurse-driven team implemented 3 interventions that led to CLABSI reduction in the PICU/PCICU:
1. Daily central line dressing audits
2. Standardization of dressing supplies in the PICU/PCICU
3. Designation and training of “dressing change champions” to perform all dressing changes
Data Collection & Analysis
• Daily audits of dressings from July 2019 - June 2020: Approximately 200 per month, for 12 months, totaling approximately 2,400 audits in one year
• Data collected on audits (included but not limited to):
• Is dressing intact?
• Is dressing up to date?
• Is dressing applied appropriately?
• Does dressing need to be changed?
• Any concerns regarding dressing?
• Monthly analysis of data collected from audits to guide QI process
• Compare PICU/PCICU CLABSI count and SIR, before and after intervention
Results
Prior to intervention, the PICU/PCICU had a CLABSI count of 6 and SIR of 1.3 in FY 2019. After intervention, the PICU/PCICU had a CLABSI count of 2 and SIR of 0.458 in FY 2020.
(see poster)
Conclusions
• Teamwork and vigilance amongst our nurse-driven, multidisciplinary team in following the interventions led to a reduced CLABSI rate and SIR in FY 2020
• Findings of this project suggest that implementing this project in your own unit may help to decrease CLABSI rate.
Limitations
• Short time frame
• Single patient setting
• Other coinciding interventions limit ability to isolate effect of dressing change interventions alone
• Unpublished UCDH data may indicate improved staff hand hygiene compliance during the Covid-19 pandemic, coinciding with data for FY 2020 Q4
Further Study
• Expand to other units
• Can the interventions be replicated?
• Would it result in a reduction in CLABSI rate?
• Are the interventions sustainable and result in continued lowered CLABSI rates?
• Will the alteration of the frequency of central line dressing audits affect the result?
• Will covert audits reflect a unit’s culture change?
References
Holzmann-Pazgal, G., et al. (2011). Utilizing a line maintenance team to reduce central- line associated blood stream infections in a neonatal intensive care unit. Journal of Perinatology, 32:281-286
Kramer, C., et al. (2019). A quality improvement approach in standardizing pediatric central venous catheter dressings and its impact on the reduction of central line-associated bloodstream infections and costs. Journal of the Association for Vascular Access, 24(2): 11-19
Wood, K.L. (2017). The impact of a team approach to central line care in preventing central line-associated bloodstream infections. American Journal of Infection Control, 45(6):S84-S85
Funding & Acknowledgements
A big THANK YOU to the PICU/PCICU multidisciplinary HAI Committee, for which this project would not be possible!

Present with Google Meet
Invite as many as 30 people, and present your poster in high definition. Transcription option is available. Free to use.
DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE