Hover to pan and click to magnify. Click again to pan at full screen.
Sydney Mullins, RN, BSN, CSSGB; David Greenhalgh, MD, FACS; Tina Palmieri, MD, FACS, FCCM; Soman Sen, MD, FACS; Kathleen Romanowski, MD, FACS; Alura Barsun, RN, MSN, FNP-C; Leonard Sterling, MBA, RN, NEA-BC; Sarah Bernardy, RN, BSN, CCRN; Marianne MacLachlan, RN, MSN, CCRN; Maureen Evans, RN; Anna Olszewski, RN, MS, CCRN; Alessandra Renteria-Turley, RN, BSN; Sarah Mattison, RN, MSN, CCRN; Kara Kidd, RN, BSN, WCC; Angela Maroon, RN, BSN
Sydney Mullins, RN, BSN, CSSGB; David Greenhalgh, MD, FACS; Tina Palmieri, MD, FACS, FCCM; Soman Sen, MD, FACS; Kathleen Romanowski, MD, FACS; Alura Barsun, RN, MSN, FNP-C; Leonard Sterling, MBA, RN, NEA-BC; Sarah Bernardy, RN, BSN, CCRN; Marianne MacLachlan, RN, MSN, CCRN; Maureen Evans, RN; Anna Olszewski, RN, MS, CCRN; Alessandra Renteria-Turley, RN, BSN; Sarah Mattison, RN, MSN, CCRN; Kara Kidd, RN, BSN, WCC; Angela Maroon, RN, BSN
UC Davis Health Burn ICU
ABSTRACT
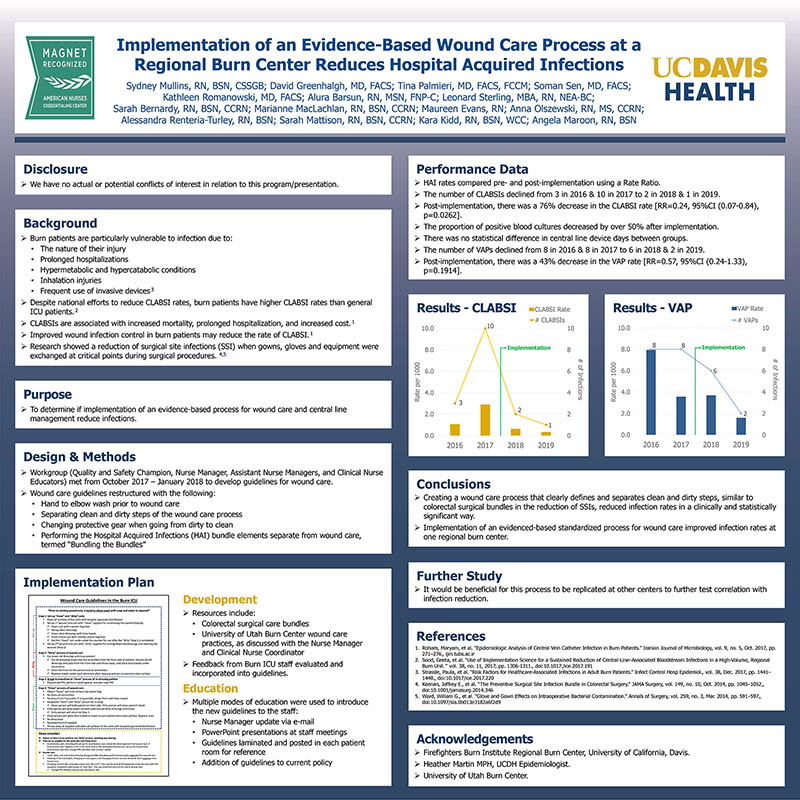
Introduction: Central line associated blood stream infection (CLABSI) rates in burn patients exceeds the national average. The purpose of this study was to determine if implementation of an evidence-based process for wound care and central line management reduce infections.
Methods: A protocol for central line and wound care was developed in conjunction with another burn center with lower CLABSI rates and a care bundle, based on colorectal surgical literature. The new protocol required hand to elbow washing prior to wound care, separating the dirty and clean steps of the wound care process, changing protective gear when going from dirty to clean and performing the Hospital Acquired Infection (HAI) bundle elements separate from wound care. CLABSI and Ventilator Associated Pneumonia (VAP) rates were then compared with the previous year.
Results: Following implementation of the new wound care guidelines, the number of CLABSIs declined from 3 in 2016 & 10 in 2017 to 2 in 2018 & 1 in 2019. Post-implementation, there was a 76% decrease in the CLABSI rate [RR=0.24, 95%CI (0.07-0.84), p=0.0262]. The proportion of positive blood cultures decreased by over 50% after implementation. There was no statistical difference in central line device days between groups. The number of VAPs declined from 8 in 2016 & 8 in 2017 to 6 in 2018 & 2 in 2019. Post-implementation, there was a 43% decrease in the VAP rate [RR=0.57, 95%CI (0.24-1.33), p=0.1914].
Conclusions: Creating a wound care process that clearly defines and separates clean and dirty steps, similar to colorectal surgical bundles in the reduction of Surgical Site Infection, reduced CLABSI and HAI rates in a clinically and statistically significant way in the Burn Intensive Care Unit.
Applicability of Research to Practice: Implementation of an evidence-based, standardized practice for wound care improved infection rates at one regional burn center. It would be beneficial for this process to be replicated at other centers to further test correlation with infection reduction.

DISQUS COMMENTS WILL BE SHOWN ONLY WHEN YOUR SITE IS ONLINE